Charley: There is no correct way to deal with carrying a BRCA gene fault

Charley, her partner and her son - shortly after birth.
After losing her mum to ovarian cancer, Charley found out she had inherited a faulty BRCA gene and had a preventative double mastectomy to reduce her breast cancer risk.
Here she shares her story so far, including the journey to having her little boy using a process called pre-implantation genetic testing, that means she avoided passing the gene fault down to him.
I lost my mum to ovarian cancer when she was 51, and I was 17. Similarly my Grandma died due to ovarian cancer around 62. I was very close to my mum, I was the youngest and her baby. Her illness and death are very hazy to me, I think I have blocked a lot of it out. I have still managed to capture some nice happy moments in my memory which I will forever cherish.

Charley and her mum.
It was only when my mum died that I became aware of BRCA gene faults.
My uncle said it would be a good idea for me to be tested. I decided to be tested for the in my early 20s, unfortunately it revealed I was a carrier. I am one of three girls and two of us carry the gene fault.
I had already decided if I were to carry the gene fault I would have a double mastectomy which I went ahead and did aged 26. The counselling involved in being tested for the gene fault is quite lengthy but I found the process ok. I think from losing my mum at such a young age, I have learnt to just get on with things and take it all in my stride. That is not to say I wasn't upset, but almost became conditioned to bad news.
I had my surgery which also involved further counselling as it is a huge decision. My double mastectomy and reconstruction went perfectly and I recovered well. I have to admit I prefer my boobs now than before, and no longer need a bra, there had to be a silver lining! I couldn't face the thought of constant monitoring and wanted to "nip it in the bud" as such. I also started a new venture during my recovery which is called Drain Dollies: I provide pretty bags to hold surgical drains post-operatively which give you a bit of dignity and also very practical.
I have been with my fiancé Tom for many years and he supported me through the entire process and has been brilliant. Life continued and we bought a gorgeous house together, got our gorgeous dog Winston and excelled in our careers.
We then started to think about having a family.
If you carry a BRCA gene fault, there is a 50/50 chance that you will pass it down each time you have a child.
I was made aware there is such a thing called pre-implantation genetic testing, or PGT-M (previously known as PGD) at Guys Hospital in London.
This is a process of IVF whereby your embryos made are screened for your genetic fault, so in my case a fault in BRCA1.
Only embryos which are not affected by the genetic condition are used and put into your womb.
This would mean you had the chance of having a child who wouldn't have to go through the same thoughts and worries as you. It is much more complicated than normal IVF.
What is PGT-M?
Pre-implantation genetic testing or PGT-M ( previously known as Preimplantation genetic diagnosis or PGD) is a special type of IVF for couples who have a risk of passing on a serious genetic condition (including BRCA gene faults and Lynch syndrome).
The process involves:
- Detailed discussions regarding the process, funding, time frame, risks and success rates
- Fertility drugs are used to stimulate egg production
- Eggs are then extracted and fertilised with sperm
- Embryos are left to develop for 2-3 days
- One or two cells are removed from each embryo and are tested to see if they carry the faulty BRCA gene
- Only embryos that are found not to have inherited the faulty gene are used
- An embryo is then transferred to the womb
There are set criteria to qualify for PGT-M on the NHS. The process from first appointment to start of treatment can be 8-18 months.
Published success rates indicate that around 1 in 3 cycles of PGT-M will result in a baby.
To find out more about PGT, who is eligible, and the centres offering it, visit Human Fertilisation and Embryology Authority website.
We decided to go for it, the process was LONG, and involved a lot of travelling. We used a satellite clinic in Sheffield and only went to London for egg collection and transfers.
Most of the time I would find myself walking the dog at 5.30am, leaving for Sheffield around 6.30 to get there for the first appointment, driving straight back to start a long day of patients in my podiatry practice. Our first egg collection yielded great results, and we ended up with 9 embryos, 6 of which were free of the BRCA1 gene fault.
We had two unsuccessful transfers. The emotions and stress were ten times greater than having a double mastectomy at 26. All the injections, drugs, travelling, time off work - and it hadn't worked.
Again, I thought why does this misery always have to happen to me. This was up until our third transfer, which gave us our amazing beautiful smiley boy Oscar, who is now 18 months old, all the heartache and stress was worth it.
He is the best little human in the world and we both absolutely adore him.
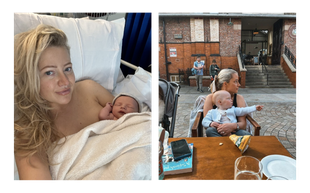
Charley and her son, Oscar.
Along with the immense happiness of having my little boy, I did unfortunately feel like I had lost my mum all over again, the one person I wanted to see this happening was her.
I have found motherhood and not having my mum around really sad at times.
Why wasn't she around to come and help me and see her grandson grow up? Why when nursery ask to fill out his family tree can there not be a photo of his beaming grandma holding him?
I know for a fact if she was here she would be very involved in Oscar’s life and he would absolutely adore her. I just have to hope she is looking down on us all and enjoying watching from above.
Along with being a busy first-time mum, the fear of ovarian cancer haunts me often, after all that is the cancer that has taken away my family members, at very young ages.
The screening for ovarian cancer is poor and not reliable, I am not under any consultants for monitoring, and I won’t ever feel "safe" until my ovaries are gone, even then I will probably still worry.
During my c-section with Oscar I did have my fallopian tubes removed at the same time.
There is evidence that a lot of ovarian cancer can start in the tubes and that removing them reduces your chances of developing the disease, so hopefully that has reduced my risk slightly. I’d like to have another baby at some point in the future, but with this in mind I also need to consider the removal of my ovaries, I think I was told around 40, I am now 35. It also isn't as simple as a double mastectomy, it's going into the menopause at 40!
Overall, I don't think there is a correct way to deal with carrying a BRCA gene fault, everyone has different approaches. I am very much a "get things done" person and that is the way I have personally navigated the process. The best thing to do is gather all the information, speak to the right people and do what’s best for you personally.
As for IVF with PGD, again this is very personal. If my mum had done it for me, I wouldn't be here. But using the knowledge and ever developing scientific research I decided it was right for me, and stop the gene fault in its tracks.
One thing I would advise for anyone considering it, is get the ball rolling, the process is LONG, the set backs make it even longer.
However, for me it has all been worth it, I couldn't have wished for a more perfect loving and happy little boy, who I hope to stick around for as long as I possibly can and fulfil all the duties to him my mum unfortunately never got the chance to.
For more information on your options when considering starting a family, see our guide to starting a family with a genetic fault.


